Author Pam Versfeld MSc (Physio) UCT, Physical Therapist Read more
The term generalised joint hypermobility (GJH) is used when a child has several joints that are more flexible than usual. This happens when the connective tissue which makes up the joint structures (capsule and ligaments) is more compliant (more easily stretched) than usual.
Generalised joint hypermobility is quite a common occurrence - in fact it is just a normal variation in the way joints are put together. Ballet dancers and gymnasts have a degree of joint hypermobility - which means that you can be hypermobile, strong, active and fit.
Yet many children with hypermobile joints have movement difficulties. Why is this and what can be done to overcome these difficulties?
Loose joints but some tight muscles
Children with generalized joint hypermobility often have some tight muscles. This can be confusing.
The muscles tightness develops because of the postures the hypermobile infant adopts when sitting on the floor. They often sit with the legs wide apart, sometimes with a flexed spine.

This leads to tightness in the muscles that cross over the back and sides of the hip and knee joints. As a result of the stiffness the child has difficulty sitting with the legs stretched forwards, may find sitting cross legged uncomfortable and has difficulty sitting erect on a chair.


Infants with joint hypermobility are often late learning to sit, crawl and walk
Infants with joint hypermobility are often late learning to crawl and may not crawl at all, instead move around on their bottoms. They are slow to pull up into standing and often only learn to walk at about 18 months.
Infants with joint hypermobility often lie, sit and stand with their hips wide apart. This leads to tightness in the hip muscles which has a long term impact on the child's motor control and is often the underlying reason for back and knee pain experienced by children with GJH.
Read more: How joint hypermobility affects an infant's development
A word about terminology
The term Joint Hypermobility Syndrome refers to a health condition which includes joint hypermobility along with pain and loss of function and as well as with several related symptoms such as fibromyalgia, anxiety, low blood pressure and fatigue.
Some people with very hypermobile joints which are unstable and may or may not partially dislocate also have a diagnosis of Ehlers Danlos Syndrome (Hypermobility Subtype). Ehlers Danlos is a genetic disorder which affects the structure of the connective tissue that holds the joint in place (joint capsule and ligaments) and connects the muscles to the bones via tendons and fascial sheaths. The poorly formed connective tissue also affects the skin which is velvety and very pliable (easily stretched).
Some medical experts do not differentiate clinically between JHS and Ehlers Danlos (Hypermobility Type). Please see the article by Tofts et al (2009) The differential diagnosis of children with joint hypermobility
A child with Ehlers Danlos should be under the care of a paediatric rheumatologist and a physiotherapist with experience in this condition.
Please note that this page provides information on children with generalised joint hypermobility. It does not apply directly to children who have Ehlers Danlos Syndrome (Hypermobility Subtype) or a diagnosis of joint hypermobility syndrome.
How hypermobility affects different joints
The elbow can be extended to form a backward angle.

The wrist can be bent so the the thumb touches (or nearly touches) the forearm.

Hypermobile fingers can be bent back to 900.

The joints in the fingers and thumbs also bend backwards.

The increased flexibility in the fingers make the hands less stable and the muscles have to work a lot harder when using the hands to grip, lift and manipulate objects.
The hips, spine and ankles are also affected by increased laxity in the connective tissue.
The legs flop out sideways when sitting flat on the floor, especially when the child is very young.

The child may have flat feet, especially if the hip muscles are tight and the ankle muscles are weak.
How is joint hypermobility diagnosed?
The Beighton scale is most commonly used measure for diagnosing generalized joint hypermobility. This a nine point scale, measuring range of motion (ROM) at 8 joints plus the ability to put the hands down flat on the floor in standing.
The recommended cut-off point for a diagnosis of generalized joint hypermobility ranges between 5 and 7 for different clinicians and researchers.
Passive dorsiflexion of the fifth metacarpophalangeal joint to < 90 degrees on the left and right hands (2 points)

Passive apposition of the thumb to the flexor side of the forearm, while shoulder is flexed 90 degrees, elbow is extended, and hand is pronated. (Add one point for each wrist.)

Passive hyperextension of the elbow 100 or more. (Add one point for each arm.)

Passive hyperextension of the knee 100 or more. (Add one point for each leg.)

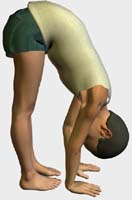
Forward flexion of the trunk, with the knees straight, so that the hand palms rest easily on the floor.
Low muscle tone and generalised joint hypermobility
Muscles are held together by sheaths of connective tissue, called myofascia, which gives them a small amount of natural stiffness. In people with joint hypermobility, these muscle sheaths are more pliable (have more give) than usual which means that the muscles have less inherent stiffness and are more easily stretched.
When a muscle contracts it shortens and develops tension. This tension is transferred to muscle's tendons and then to the bones to produce movement. In joint hypermobility the transfer of tension from the muscles the bone is less efficient. This means that the muscles have to work harder to produce movement and provide stability.
The myofascial sheaths that hold the muscle together also give muscles the feeling of firmness when palpated. In joint hypermobility the laxity in the myofascial sheaths makes the muscles feel floppy.
It is important to understand that the low tone which is seen in joint hypermobility is caused by the structure of the muscles themselves.
The only way to improve the tone in muscles with lax connective tissue is by strengthening the muscle which will increase the stiffness in the connective tissue that forms the tendons and myofascia.
Hypermobile joints are easily injured
Children with joint hypermobility, muscle weakness and possibly poor coordination are more likely to complain of pain and tiredness and are more likely to suffer from joint sprains, leg pain and night pain..
The laxity in the joint ligaments make them more vulnerable to injury. Weak muscles are less able to able to protect the joints during during everyday activities that require a degree of fitness and agility.
Joint injury and pain can be reduced by strengthening weak muscles, increasing flexibility of tight muscles and improving coordination.
Read more: How do I know if my child has weak muscles?
What causes joint hypermobility?
The degree of compliance (stretchiness) in connective tissue is genetically determined. Between 10 and 20% of people have connective tissue that is more pliable ( less stiff) than usual. So some degree of joint hypermobility can be viewed as part of the normal variation in the structure of the connective tissue within the population.
Children with generalised joint hypermobility will usually have a parent or other close relative with hypermobility.
Having hypermobile joints is often seen as a plus factor, particularly in gymnastics and ballet dancing. To be a ballerina you need to have some degree of hypermobility.
Hypermobility is also not always associated with movement difficulties. In my experience as a children's physiotherapist, it is the combination of hypermobility, weakness, some muscle tightness and a very cautious nature that leads to movement difficulties.
Postural and movement difficulties children may have
Children with GJH often have difficulties with a range of everyday, classroom and playground tasks and activities. Poor general fitness along with muscle weakness and tightness in some muscles contribute to these difficulties especially if the child has a cautious nature and avoids tasks that require physical effort.
Children and adults with joint hypermobility well to fitness training aimed to increase strength and stability, stamina and participation in sport activities. The secret is to start slowly and gradually increase the training demands (strength, stamina, endurance, coordination) the individual is able to participate in games in the playground and sport activities.
Ideally, and especially if a child has pain and joint instability, any exercise program should be overseen by a physical therapist with a special interest in joint hypermobility. However, many children with generalized joint hypermobility just need some extra encouragement to work hard at getting fitter. The SfA Online Fitness and Coordination Guide has many ideas for helping children to develop basic levels of strength and stamina.
Generalised joint hypermobility and flat feet
Many children with joint hypermobility (low muscle tone) have problems with flat feet. The inside border of the foot does not have a good arch and the heel bone is often angled outwards.
In addition children with flat feet often stand with their feet turned out, and sometimes with the feet far apart. This tendency to stand with the feet turned out and far apart places abnormal stresses on the feet and hinders effective push-off for walking, jumping and running. Read more: Flat feet; not just a foot problem

Generalised joint hypermobility is associated with a range of physical difficulties
The increased compliance in the connective tissue that causes hypermobility in joints also affects other parts of the body leading to a number of problems, including:
- Bladder problems and bed-wetting
- Bladder infections and vesicoureteral reflux
- Low blood pressure
- Esophageal reflux
- Chronic fatigue
- Chronic pain
- Idiopathic scoliosis - especially in girls where there is a family history of scoliosis
Children with joint hypermobility often complain of leg and back pain
The combination of loose joint structures (ligaments and capsule) along with muscle weakness and some tight muscles causes abnormal stresses on knee joints which in turn leads to knee pain after exercise or at night. More about leg pain
Children with joint hypermobility may also experience back pain due to poor posture and muscle weakness.
New Graded strength exercises for children who complain of leg pain
SfA Fitness and Coordination Training Guide
All the information you need to be your child's coach and advocate
$10 for subscription
Subcribe here
|
Includes |
Disclaimer The content on this site is provided for general information purposes only and does not constitute professional advice. All liability is excluded to the fullest extent permitted by law in respect of any loss or damage whether direct, indirect or consequential that arises in connection with the use of or reliance upon any content forming part of this site.</

